Gastropersis How Do You Know When Your Stomach Starts to Work Again
Click here to download a PDF of this information.
Gastroparesis

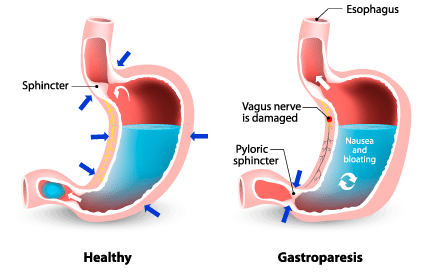
The term 'gastro' refers to the stomach, and 'paresis' means fractional paralysis; therefore, gastroparesis ways partial paralysis of the tum. To empathize what goes incorrect in gastroparesis, information technology is important to know how a healthy digestive tract functions. When nosotros swallow, we start past chewing and swallowing (ingesting), which requires conscious try. One time the food reaches the esophagus, an automatic, rhythmic motion (peristalsis) takes over, propelling the contents all the way through the digestive tract. Typically, the passage of nutrient from one area of the digestive tract to the side by side is precisely coordinated, so that food stays in each area for just the right amount of time. For the stomach, this is approximately ii hours.
However, in those with gastroparesis, the food does not move from the stomach into the intestine as rapidly equally it should (delayed gastric emptying). Gastroparesis is a movement disorder, which means at that place is no concrete obstruction preventing timely digestion, but rather a trouble with muscular activity regulation. It occurs when the pair of fretfulness that connects the brainstem to the alimentary canal (vagus nervus) is damaged or not functioning properly. Since the vagus nerve is unable to transport the necessary letters to ensure that the muscles in the stomach go along to work normally, nutrient remains in the stomach for too long, leading to symptoms.
Causes of Gastroparesis
The most common cause of gastroparesis is diabetes mellitus blazon 1 or type two. High levels of glucose in the blood tin cause chemical changes to the vagus nerve. This type of gastroparesis tin be especially dangerous, considering the delayed gastric emptying leads to more than intense claret sugar spikes in those with diabetes, causing a cycle of claret carbohydrate highs and lows that continues to bear on the vagus nerve.
Gastroparesis is typically associated with some class of damage to the vagus nerve, which tin can occur in a range of situations, including from various mineral deficiencies, eating disorders, opioid medications, sure antidepressants, and surgeries in the upper alimentary canal, such every bit gastrectomy or bariatric surgery. Other causes of gastroparesis, although very rare, include connective tissue diseases such as scleroderma and Ehlers-Danlos syndrome, and neurological conditions such as Parkinson'south disease. In about a third of cases, the cause of gastroparesis is unknown (idiopathic). In some cases, such as those caused by certain medications or eating disorders, the gastroparesis tin be temporary, with normal digestive function returning upon medication aligning or adapting to healthy eating habits.
Prevalence of Gastroparesis
Gastroparesis affects approximately iv% of the population and is more common in women. Many people with gastroparesis also have diabetes, and fifty% of those affected had diabetes before the onset of their gastroparesis.
Gastroparesis Symptoms & Complications
The about common symptoms of gastroparesis include feeling full from small amounts of food, nausea, airsickness, reduced ambition, intestinal pain, heartburn or gastroesophageal reflux disease (GERD), and regurgitation. These symptoms can lead to weight loss and food deficiencies. Other symptoms include bloating, muscle weakness, and night sweats. Since the digestive organization doesn't work smoothly, those with the condition besides experience periods of low blood saccharide while the food remains in the tummy, and high claret sugar when it eventually reaches the intestines.
Sometimes, more severe complications tin occur due to delayed gastric elimination. Individuals can experience obstructions caused by masses of solid hardened food (bezoars). Oft, bezoars will pass on their own, but other times they require treatment in the grade of oral solutions to assist dissolve them or, in severe cases, surgery.
If excessive vomiting is a symptom, it can cause its own fix of complications, including dehydration and malnutrition. In those who have diabetes and gastroparesis, decision-making claret carbohydrate can go very difficult due to the irregular release of food into the modest intestine.
Diagnosing Gastroparesis
Your physician will review your symptoms and medical history and complete a concrete examination, including blood tests. If he or she finds it likely that you take gastroparesis or is unsure and wants to rule out other diseases and disorders, there are a few tests bachelor. This is particularly of import with gastroparesis, because many of the symptoms are similar to other disorders, such as functional dyspepsia.
Gastric elimination scans permit your healthcare team to measure the speed at which y'all digest food. For this exam, you lot eat a tiny amount of radioactive textile with a small-scale meal, which allows technicians to monitor the rate at which information technology passes through your digestive organisation by periodically using a photographic camera to cheque where the radioactive repast is. If information technology stays in the tum for also long, then it can indicate gastroparesis.
An upper gastrointestinal series involves consuming a barium drink in front of an x-ray machine afterward fasting. The barium is a chalky liquid that shows up on ten-rays, allowing the technicians to run across details in the gastrointestinal tract. This can assist them find any anomalies in tum function.
Gastroscopy involves a physician using a modest, flexible tube with a camera and a lite (endoscope) to look at the upper parts of the digestive system, including the esophagus, stomach, and duodenum. This test is helpful to find bezoars or whatsoever other abnormalities in the stomach.
Abdominal ultrasound is useful for identifying if there are any physical abnormalities that might exist causing symptoms.
Gastric or duodenal manometry involves using a long sparse tube that measures muscle strength and patterns inside the esophagus and through the lower esophageal sphincter into the stomach.
Management of Gastroparesis
The management of gastroparesis tin include simple dietary changes, medications, and even surgery depending on the affliction severity.
Lifestyle and Dietary Changes
In individuals with mild gastroparesis, a few changes to dietary habits can largely reduce symptoms. Near of these changes focus on reducing the amount of nutrient y'all swallow at once, considering overeating makes information technology fifty-fifty more than difficult for your stomach to empty. Consuming smaller meals more frequently, rather than ii or three large meals, tin help. You may also discover relief by eating mostly soft or liquid foods, such as soups and smoothies. Chewing each bite very well and consuming non-fizzy liquids with meals can also make digestion easier. Avoiding or limiting loftier fibre and high fatty foods can reduce discomfort, since these foods typically accept longer to digest. For some individuals, supplemental nutrition beverages tin assistance ensure adequate nutrient intake.
If you take diabetes, make sure to go on glucose tablets or difficult candies on paw. Y'all can use them to raise your claret sugar, because they are easily captivated, if gastroparesis is causing low blood sugar. A registered dietitian can offer advice if you are unsure what to swallow then that y'all encounter your diet requirements when you have gastroparesis.
Medications
The medications available for gastroparesis don't treat the underlying disease, but they help to alleviate symptoms. At that place are ii primary medication types available:
Motility agents increment the speed of peristalsis, causing the tum to empty more quickly, and include metoclopramide (Reglan®, Maxeran®) and domperidone (Motilium®). NOTE: Wellness Canada pulled a gastroprokinetic agent, cisapride, from the market at the turn of the century due to serious health concerns and deaths. Nevertheless, some physicians still cautiously prescribe cisapride, which increases motion in the upper gastrointestinal tract, for severe cases of gastroparesis. Compounding pharmacies can acquire the drug under special circumstance.
Antiemetics reduce nausea and airsickness, and include medicines such as prochlorperazine and promethazine.
Surgery
For those who are unable to get symptoms under command through dietary changes and medications, in that location are a few surgical options that may offer relief.
A gastric electrical stimulator is an implanted device that uses balmy, controlled electrical pulses to stimulate the smoothen muscles in the digestive tract and speed upwards gastric elimination. However, this treatment does non work for anybody, and is not available in all areas.
Botox (botulism toxin) injected in the sphincter that connects the stomach to the small-scale intestine (pylorus) tin help relax the sphincter so that it more easily allows food passage into the small intestine. Botox injections don't work for everyone, they are merely a temporary solution, and can become less effective in subsequent injections.
A feeding tube surgically attached at the entry to the small intestine can offer a last resort for those who are completely unable to take nutrients into the stomach in either solid or liquid grade.
Gastroparesis Outlook
Gastroparesis is typically a chronic condition with potentially dangerous side furnishings. For some individuals, being more than conscientious virtually the frequency and types of foods they consume is plenty to live a relatively normal life, but for others, ongoing medications and even surgery might exist necessary. Quality of life is oft diminished with gastroparesis. Those who have both diabetes and gastroparesis need to be especially diligent.
Want to Larn More?
- Gastroparesis Story
- Gastroparesis Patients Willing to Take Massive Risks for Cure
- Diabetes and the Gut
Paradigm Credits (elevation to bottom): © bigstockphoto.com/Ammentorp, © bigstockphoto.com/designua
Source: https://badgut.org/information-centre/a-z-digestive-topics/gastroparesis/

0 Response to "Gastropersis How Do You Know When Your Stomach Starts to Work Again"
Post a Comment